85% of the global population lives in cities and human settlements*
making the health of cities and human settlements and the impact it has on people and the planet,
the greatest shared responsibility of our time.
The Global Urban Systemic Health Partnership is a transdisciplinary global knowledge network at the interface between science and action. We believe that a sound knowledge of a city’s health condition is necessary for them to thrive and respond to the challenges of global changes. We support cities and human settlements in assessing their overall health condition and unleashing their potentials to stay fit for the future.
Urban systemic health is the resilience and potential of an urban community to adapt or transform in response to change.

Unlocking the
SYSTEMIC
HEALTH
potential of cities and human settlements
Building urban resilience through systemic health – maximizing co‑benefits when funds are tight.

is about the immunocompetence of cities and human settlements - their ability to function, adapt, transform, to self-organise, self-create (autopoiesis), and be resilient for people and the planet.
Urban Systemic Health
The urban immunocompetence is based on the ability of a complex system to self-organise, respond to change and adapt.
The sustainable development dilemma is a result of trying to ‘create more with less’, without understanding the complexity. The naive idea was that economic growth must be decoupled from environmental degradation and pollution in an ever accelerating race for efficiency enhancing innovations. That is naive because it only works in very specific urban complexity conditions.
The attempt to improve human health and wellbeing in cities becomes flawed when the health costs of doing so outweigh the benefits - even and especially when those costs are externalised. The sustainable development dilemma is then created due to negligence and ignorance of the systemic health capacity of cities.
The conventional development model only works well during certain stages of urban complexity development. After that, progress measures must be adjusted to what we value. If not, social and environmental externalities (costs) are created that harm people and the planet. It becomes too expensive to be poor and unhealthy.
Discovering and tapping into the systemic health capacity of cities can unleash enormous potentials for sustainable development. By discovering synergies, co-benefits and the connective intelligence of cities, renewable potentials of cities can be unleashed that make them thrive.

Urban planet
Most of the world's population lives in cities and is exposed to unhealthy levels of air pollution, contributing substantially to non-communicable disease burdens and leading to 1.8 million excess deaths in 2019.
Local data on the systemic health conditions of cities are urgently needed to act.
In 2025, approximately 4.8 billion people, or 58% of the global population (8.2 billion), lived in cities.
This number is expected to continue to increase, with projections indicating that around 68% of the world's population will live in urban areas by 2050.
Cities are responsible for about to 70% of global CO2 emissions associated with energy consumption. Between 2000 and 2019, studies estimate approximately 489,000 heat-related deaths occurred each year, with 45% in Asia and 36% in Europe.
As of 2024, 58% of the world’s population live in urban areas and this is set to rise to 68% by 2050**.
Almost 40% of urban dwellers have no access to safely managed sanitation services and many lack access to adequate drinking water.
An estimated 91% of people in urban areas breathe polluted air.
Poorly designed urban transport systems create a range of threats including road traffic injuries, air and noise pollution and barriers to safe physical activity – all leading to higher levels of noncommunicable disease and injuries.
Continued urbanization is expected to lead to cities becoming epicentres of disease transmission, including vector-borne diseases.
Under current urban population growth in cities, the potentially global urban area will grow 3-fold by 2030.
Despite covering only about 3% of the Earth's land surface, urban areas are responsible for approximately 75% of global energy consumption.
Cities are 2-10 degrees celsius hotter than rural areas. Without adaptation, heat deaths could rise 370% by mid-century. Althouth life expectancy is higher in cities and health care facilities tend to be better than in rural areas, urban lifestyles and non-communicable diseases account for over 70% of global deaths, and the burden is increasingly urban.

Regular urban health checks will better inform planning and decision-making
Urban systemic health checks are still rare and irregular—yet cities are changing faster than ever.
Urban populations are growing and health disparities are widening. Occasional assessments are no longer enough to keep pace with the speed and scale of urban transformation.
This new partnership aims to increase both the frequency and quality of urban health diagnostics—so that city leaders can act faster, smarter, and with greater confidence.
This partnership leverages a robust, science-based methodology to provide timely and actionable insights into the systemic health of cities.
With these tools, decision-makers can track vulnerabilities, identify co-benefits, and prioritize integrated actions—turning complexity into opportunity for healthier, more resilient urban futures.
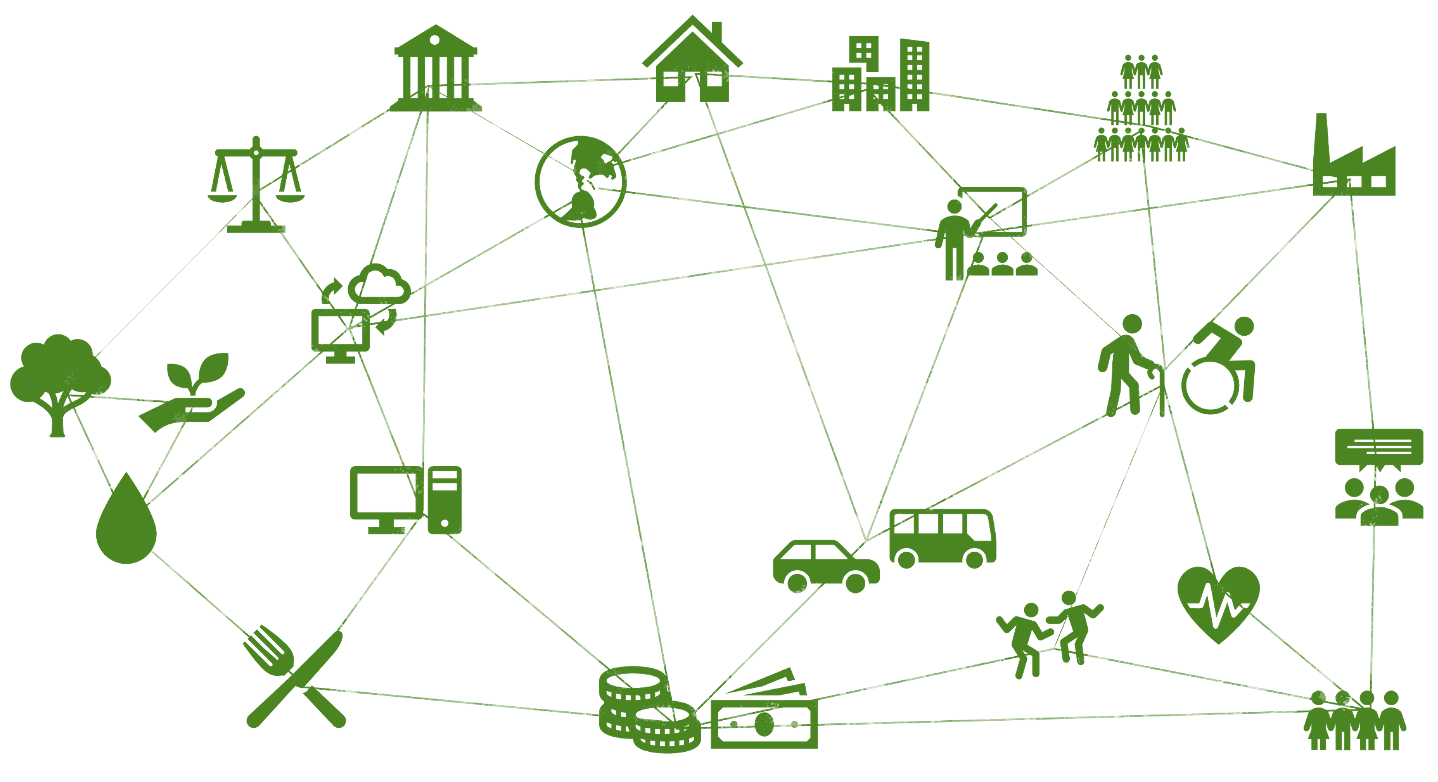
Cities are complex adaptive systems
Cities and human settlements play a central role in balancing human wellbeing and planetary health
and they can do that by unleashing their urban systemic health capacity.
The complexity of cities and human settlements is an untapped hidden renewable resource for creating urban advantages and advancing health and wellbeing.
Understanding urban complexity is the key to solving urban health challenges, despite financial shortages of urban communities.
Ignorance towards urban complexity has led to premature urban economic decline and environmental degradation.
The dilemma of sustainable development is that human wellbeing has come at the expense of planetary health.
How it began
Dr. Franz Gatzweiler is founder of the Global Urban Systemic Health Partnership. He was executive director of the International Science Council’s global science programme on Urban Health and Wellbeing: a Systems Approach from 2014 - 2022; science advisor at the United Nations University Institute for Data and Digital Technologies in Macau in 2023 and consultant for the Institute of Urban Environment, Chinese Academy of Sciences in 2024. From 2004-2014 he was senior researcher at the Center for Development Research (ZEF Bonn), University of Bonn, Germany where he is a senior fellow to date. He is a member of the IAP working group on Urban Health and Well-Being. His PhD dissertation was “on the nature of economic value and the economic value of nature” and he did his habilitation in the field of resource economics, on the topic of “an economics of living systems”.
Prof. Pierre Ritchie was the first chair of the International Science Council’s global science programme on Urban Health and Wellbeing: a Systems Approach.
Together with a team of international and interdisciplinary professionals from public, global, population health, geography, epidemiology, computer science, architecture, urban science and design, economics and social sciences, Gatzweiler proposed a new urban health science which merges natural and social science approaches, in particular the new science of cities, development economics, complex systems science, and health sciences.
Pierre Ritchie
It all began with the decision of the ISC, the International Science Council, to establish a global science programme on “Urban Health and Wellbeing: a Systems Approach”.
The systems approach was still not science mainstream and came at a time when ISC began its merger with the International Social Science Council (ISSC) and continued its promotion of a post-normal, transdisciplinary, mission-oriented science.
Over the course of 10 years, a major shift in the scientific understanding and approach to urban health and wellbeing occured; documented in the three science plans:
We started by emphasizing the application of systems analysis and modelling approach to urban health and wellbeing issues. The underlying model tended to be anthropocentric and deterministic. That model of urban health saw people in cities at the center, whose health is influenced by multiple proximate and distal determinants. By understanding the systemic interrelationships of the determinants, so was the assumption, we would know better how to improve the health and wellbeing of people in cities. The idea was that by adjusting the systemic interconnectivity of cities they could become better and more efficient at improving human health and wellbeing. That type of “systems approach” was still deeply rooted in the conventional positivistic scientific method, assuming that a complex urban system can be fully understood, managed, controlled and adjusted if sufficient data were available. The definition of urban health was about the health of people living in cities. In contrast, our understanding of urban (systemic) health is that it is an emergent property of complex urban systems.
It soon became evident that the global Sustainable Development Goals (SDGs) were not going to be achieved by 2030.
Although poverty was reduced, life expectancy increased and infant mortality was considerably reduced, the conventional anthropocentric development paradigm was still in use and did not halt the detrimental effect it had on planetary health.
Deteriorating planetary health had negative impacts on human health in cities. The anthropocentric approach could not address the dilemma that cities could improve human health and wellbeing, but at the costs of planetary health. According to that model, cities were merely a means to the (short term) end of improving human health and wellbeing. Cities which achieved that goal, especially cities in developed nations, were not healthy for the planet, due to their ecological footprint which exceeded the global biocapacity.
Fuders argues that the current monetary system, with its inherent growth imperative, contributes to unsustainable practices that adversely affect urban environments and public health. The growth paradigm only leads to healthy outcomes in certain stages of complexity development. By reimagining the role of money, he suggests that economies can shift towards models that prioritize ecological balance and social well-being, which are essential components of urban health.
The pursuit of health and wellbeing for people alone has transgressed biophysical boundaries and the planet’s biocapacity - that is the capacity of ecosystems to provide goods and services, which keep the urban system thriving.
The diagram below, by the Global Footprint Network shows that countries with a high human development index, like the EU countries with a red circle, has come along with an ecological footprint that is too large to be sustainable, and progress has come with transgressing biophysical capacities.
The diagram by O’Neil et al. 2018 (above) shows that achieving social goals seems to come with transgressing biophysical boundaries. Ideally most countries would be in the green square in the upper left corner.
That situation urged us to think of a new approach to urban health and wellbeing, one which puts cities center stage and looks at the systemic health of cities: their ability to balance human and planetary health, to adapt to change and systemically transform.
The new transdisciplinary systems approach to urban health and wellbeing was written in that spirit co-authored by an international scientific committee put together by the International Science Council.
The old model of cities sees them as nodes of a globally interconnected system; places that evolved from extracting energy and resources from their proximal and distal environments by land, water and air; places of negentropy which flourished, became increasingly complex and provided for the health and wellbeing of their inhabitants. That is valid for a certain period of urban complexity development. The new urban systemic health model perceives cities as complex living, social-, ecological-, technological systems, capable of self-organisation and self-creation (autopoiesis) beyond central planning and control. It is precisely that capability which can enable urban communities to unleash their urban systemic health capacity, become resilient and strengthen the urban immunocompetence.
Systems approaches are needed
A key message of the LANCET Pathfinder commission 2023 is:
“Systems approaches are needed; achievement of transformative change across sectors to achieve improved health equity at net-zero greenhouse gas emissions requires systems approaches that integrate adaptation and mitigation and address underlying structures driving inequity and rising greenhouse gas emissions. Examples of implemented and evaluated transformative action are urgently needed to inspire and inform change.”